Burnout often results from extended periods enduring the emotional stress precipitated by unaccomplished expectations or failure to fulfill unreasonable demands. The symptoms can include intensified emotional exhaustion, physical fatigue, lowered self-worth, changes in eating and exercising habits, social withdrawal, sleep disorders, anxiety, and depression.
If You’re Burned Out, Your Brain Has Rewired to Survival Mode
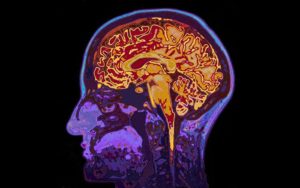
There are specific and reproducible patterns of changing neural activity and brain connectivity associated with the stress buildup that leads to burnout. In the high-stress state subjects’ neuroimaging scans reveal less activity in the higher, reflective brain (Prefrontal cortex/PFC) and more activity in the lower, reactive brain that controls involuntary behaviors and emotional responses. Prolonged stress correlates with structural increases in the density and speed of the neuron-to-neuron connections in the emotion-driven reactive networks of the lower brain and corresponding decreases connections in prefrontal cortex conscious and reflective control centers.
The explanation of these changes is attributed to the brain’s neuroplasticity defined by the phrase: “neurons that fire together, wire together.” The brain literally rewires to be more efficient in conducting information through the circuits that are most frequently activated.
When stress is frequent, the more frequent activation of the neural pathways to the lower, stress-reactive brain results in their strengthening from enhanced wiring (dendrites, synapses, myelinated axons). These pathways can become so strong that they become your brain’s fast route to its lower, reactive control centers. The stressful, burned out state when the lower, reactive brain is in charge overcomes the calm, reflective, and productive higher neural processing in the (PFC) – the preferred brain locale for control of behavior and emotional self-management.
As your efforts to achieve unreasonable goals are thwarted or increasing demands recur, and the lower brain dominates more frequently, you lose touch with your reflective brain. With less management coming from your reflective PFC, it becomes harder and harder to logically see these challenges in realistic perspective or to solve problems creatively.
Disappointments take on more emotional power and without your higher brain’s perspective, they are interpreted as personal failures. Your self-doubt and stress further activate and strengthen your brain’s involuntary, reactive neural networks. The spiral down to burnout accelerates as these circuits become the automatic go-to networks. Your brain achieves less success in problem-solving and emotional control and ultimately reacts by withholding efforts to escape the burnout state.
Reset Your Brain’s Default Neural Network from Retreat to IGNITE!
The good news is you can apply what we’ve learned from neuroscience about your brain’s survival mode to take actions to retrieve voluntary control of your choices and emotional wellbeing.
You can activate the same neuroplasticity, that gave dominance to the lower brain networks in the burnout state, to construct a new, stronger positive default response. With increasing successful experiences in achieving goals, you can reset the circuits to redirect your brain to access its highest cognitive resources. You can build up newly improved circuitry switching your responses from retreat to IGNITE for mindful awareness and creative problem-solving!
Since an effort-failure pattern sets up the brain’s survival response to withhold effort, you’ll need to strengthen your brain’s recognition that effort toward your goals can result in success. Your weapon of mass reconstruction can come from your brain’s very powerful drive for its own intrinsic neurochemical reward— dopamine and the deeply satisfying and motivating pleasure it brings. When the brain releases dopamine in rewarding bursts, you experience a deep intrinsic satisfaction along with increased motivation, curiosity, perseverance, and memory. Dopamine is particularly released when your brain recognizes that you’ve achieved a challenge (from the “I get it” of figuring out a joke to the satisfaction of completing a marathon).
To get the dopamine-pleasure response from challenges achieved, you’ll need to plan for your brain to experience frequent recognition (feedback awareness) of incremental progress. The choices of what you set as a goal should be guided by their desirability and the goal’s suitability to be broken down into clear segments. You want to set goals, the progress of which, you can chart or easily recognize with each stepwise challenge and success. The pleasure burst of dopamine’s intrinsic motivation accompanying your brain’s recognition of each progressive increment achieved in the goal pathway will keep you motivated to persevere.
Goal Buy-In for Your Brain’s Neural REWIRING
Buy-in and relevance are important in choosing your rewiring goal. Since your goal is to rewire your brain’s expectations that your goal efforts do yield progress, despite increasing challenge, you need to really want the goal. This is not the time to challenge yourself with something you feel you should do, but won’t really look forward to, such as dieting, climbing stadium stairs, or flossing after every meal.
The idea of planning and achieving goals as a burnout intervention is probably not new to you. These are likely to be activities you’ve considered but didn’t do for the obvious reason. They take time. when it comes to adding another activity to your schedule, past experiences have left you with the expectation that there is not enough time.
These first goals that can provide ongoing awareness of your progress are often tangible (visible, such as planting a garden or making pottery on a wheel, or auditory such as playing an instrument, or physical such as learning tai chi), but your goal can also be spending more time at something you already do, but want to do more frequently or successfully, such as journaling, practicing yoga, or sketching.
You’ll Find Your Own Goal for Buy-In, but Here are Some Examples of Planning
Physical goals: Notice I didn’t say exercise. That’s not as motivating as “training” for a physical goal you want to achieve, even though they often overlap. If you want to run a 10K, and you enjoy running, the goal for an achievable challenge could first be building up to the distance starting with your baseline distance you comfortably run now. Then, plot out the increments that you’ll consider progressive successes, such as adding 100M each day or a week (with increments based on what you consider both challenging and achievable). Once you reach 10K goal, speed can become the next goal again plotted out in segments of incremental progress before you start.
Hobbies: From woodworking to shooting wooden arrows, hobbies really are opportunities for brain rewiring. Again, plan your stepwise achievable challenge increments. If you select darts, start with a home dartboard—low initial investment and throw from a close, but challenging distance at first. As you get better in accuracy move back further. Record your results with the notations of the distance of each improvement you set as an achievable challenge. If you get so good that you are no longer challenged by the dartboard, try that archery!
Mindfulness and meditation are certainly positive interventions for burnout and will be topics of a subsequent blog.
Your Rewired Brain’s Default Changes from Defeat to Ignite
With your understanding of what happened in your brain to create the hopeless frustration of burnout, you’ll hopefully have more positive expectations to help you put in the effort to try (or retry) suggested interventions. Your own natural dopamine-reward system will then be at work deconstructing the resistance network built by your burnout as you reset your circuits of motivation.
The repeated experiences of dopamine-reward you’ll experience as you monitor your goal progress will literally change your brain’s circuitry. Repeated effort-reward experiences promote the neuroplasticity creating neural networks that expect positive outcomes in your new default network. This is because your brain will build stronger connections into the memory pattern. The expectation in achieving this challenge will bring pleasure. As with other less used networks, the previous lower brain stress-activated go-to response network you developed in burn-out, that caused you to react negatively to stressors, will be pruned away from disuse.
You’ll be rewired with optimism and renew positive expectations about your self-efficacy. With your higher, reflective brain back in control, as you access your perseverance, innovation, and creative problem-solving when you need them.
Just be sure to take the time to break down big challenges into opportunities to recognize incremental progress as you achieve each small step en route to your goals. With that positive recharge, your well-deserved dopamine reward will sustain your brain’s motivated perseverance on to the next step of the path to your goals.
Dr. Judy Willis is a board-certified neurologist and middle school teacher, specializing in brain research regarding learning and the brain. With a unique background as both a neurologist and classroom teacher, she writes extensively for professional educational and parenting journals and has written six books about applying the mind, brain, and education research to classroom teaching and parenting strategies. The Association of Educational Publishers honored Dr. Willis as a finalist for the Distinguished Achievement Award for her educational writing. Check out her website.






 Think of something you’ve always wanted to do or be good at, and then identify manageable steps that you can take on a consistent basis that gradually takes you towards your goal. Don’t say I need to be as good as someone else or make an arbitrary benchmark-rather say I want to get in better shape relative to how I am right now, so I’m going to run or go to yoga more often. Or I’ve always wanted to know how to tie my flies, shuffle a deck of cards, play an instrument, or speak a foreign language, so I’m going to work on this task a few minutes each day as opposed to watching TV or surfing the web.
Think of something you’ve always wanted to do or be good at, and then identify manageable steps that you can take on a consistent basis that gradually takes you towards your goal. Don’t say I need to be as good as someone else or make an arbitrary benchmark-rather say I want to get in better shape relative to how I am right now, so I’m going to run or go to yoga more often. Or I’ve always wanted to know how to tie my flies, shuffle a deck of cards, play an instrument, or speak a foreign language, so I’m going to work on this task a few minutes each day as opposed to watching TV or surfing the web.







 Robin Williams’ death – like the death of so many others by suicide who have suffered from severe mental illness – issued from an unsound mind afflicted by a devastating disorder. Depression affects not just a person’s moods and emotions; it also constricts a person’s thinking – often to the point where the person feels entirely trapped and cannot see any way out of his mental suffering. Depression can destroy a person’s capacity to reason clearly; it can severely impair his sound judgment, such that a person suffering in this way is liable to do things, which, when not depressed, he would never consider. Our Lord’s ministry was a ministry of healing, in imitation of
Robin Williams’ death – like the death of so many others by suicide who have suffered from severe mental illness – issued from an unsound mind afflicted by a devastating disorder. Depression affects not just a person’s moods and emotions; it also constricts a person’s thinking – often to the point where the person feels entirely trapped and cannot see any way out of his mental suffering. Depression can destroy a person’s capacity to reason clearly; it can severely impair his sound judgment, such that a person suffering in this way is liable to do things, which, when not depressed, he would never consider. Our Lord’s ministry was a ministry of healing, in imitation of 
 Have you ever felt so stressed out and overwhelmed that you can’t think straight? We now know that prolonged
Have you ever felt so stressed out and overwhelmed that you can’t think straight? We now know that prolonged