Depression is a state of shutdown in which an individual’s psychological system shifts toward negative feeling states and diminishes the positive feeling states. The hallmark features of a depressive episode is a high negative mood state (characterized primarily in terms of depressed/demoralized/defeated/despairing feelings and secondarily in terms of anxiety, irritability/defensive hostility, and guilt/shame) and a diminished positive mood state (loss of interest, pleasure, energy, desire, and excitement).
Why do people get depressed? The primary reason people enter depressive shutdowns because they cannot obtain the necessary psychological nourishment needed to energize their behavioral investment system. Think of it as being akin to a state of starvation, only instead of physiological nutrition, the individual is lacking psychological nutrition. What is psychological nutrition? The fundamental principle that underlies psychological organization is that of behavioral investment. The psychological system is organized to direct mental energy and action toward investments that offer a return on those expenditures. When one is a getting a good return on one’s investments, then one feels fulfilled, energized and engaged. However, when one is not getting a good return, one begins to feel frustrated, anxious, irritable, or disappointed. If one cannot find an effective pathway for getting one’s needs met, one begins to enter into a state of psychological shutdown called depression.
So what are the core psychological needs that people have that need to be nourished? There are many different possible classification systems of needs (and motives and goals that people seek fulfillment around, see, e.g., here). I offer five categories here that overlap loosely with Maslow’s classic hierarchy of needs.
Safety and Security Needs. First and foremost, the psychological investment system is concerned with basic safety and survival. If one’s physical safety is chronically threatened, if one is in constant pain, if one is chronically hungry, and so forth, the attention of the system will largely be focused here.
The Base Pleasures. Good sex, tasty food, relaxing on a warm summer day on the beach after working hard. The “hedonic” pleasures serve as a fundamental reward and signal positive investments (at least in the short term). Good investment systems are generally characterized by meaningful effort and hard work toward a productive goal, followed by short periods of relaxing and enjoying the base pleasures.
Relational Needs. Our core psychosocial need is to be known and valued by important others. Most notably, this includes being known and valued by members of our family of origin, friends/peers, romantic partners, and community. Needs for relational value are reflective of one’s degree of social influence. And folks go about achieving social influence and relational value in different ways. For example, see here for power and achievement needs relative to belonging and intimacy needs.
Developmental Growth Needs. We can think about an individual’s psychological system as being akin to an investor’s portfolio. An investor has resources that have the potential for growth and loss. An investor with a diverse portfolio whose investments are growing in a way that is exceeding expectation is flourishing. The same is true for an individual. Each individual will have “personal projects” that are engagements they are involved in that afford opportunities for growth (hobbies, interests, creative and playful endeavors, meaningful work projects, etc.). If an individual is chronically stuck and not growing or is largely cutoff from their growth pathways, or is frequently failing to meet expectations, or is deeply investing in pathways based on extrinsic reasons that are not consistent with their underlying emotional/motivational needs (or intuitive sense of potential), then the investment system is vulnerable.
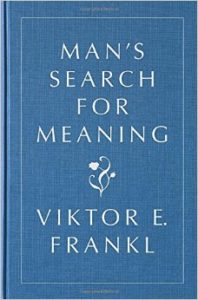
Existential/Transcendental/Virtuous Needs. Adult humans are meaning-making creatures that need to have a narrative for how their lives and personal projects make sense. As Victor Frankl notes in his timeless classic Man’s Search for Meaning, if they cannot place their suffering, personal projects, virtues and relationships in the context of a larger narrative that provides meaning, then they will be vulnerable to developing a nihilistic attitude, which is the belief that their lives or actions really don’t matter, because really nothing matters. A nihilistic narrative can undercut the emotional value that folks get from engaging in such projects, leading to existential crises or depressions.
Why do people have trouble getting their psychological needs met? Sometimes the answer is obvious. For example, consider the city of Aleppo in Syria. The people of that city have been completely brutalized and many folks there undoubtedly feel depressed. (As an interesting aside, it is worth noting that the field of psychiatry/clinical psychology is divided as to whether such individuals should be considered “clinically depressed”). In other obvious cases, folks get depressed because of chronic pain or illness, or death of a loved one or because they get addicted so substances that ruin their lives or because they are abused or isolated.
Other times the issue is much more complicated. Consider that there are many people that live in nice houses and seem to be surrounded by caring people and are achieving in their lives, yet they also get depressed. Indeed, despite the fact that we have more and more technology and more and more resources and control over our environment, we seem to be struggling more than ever with feelings of depression and anxiety. What is going on in these cases?
The short answer is that I think the modern, fast-paced society is placing many new, unusual stressors on our emotional system. And I don’t think people have been well-educated about how to appropriately process negative feelings. People have been given much more freedom to acknowledge negative feelings than in past generations (read this story to see what I mean), but there has not been good education on how to learn and grow from such feelings (see here or here). What I see in my clinic is that individuals try to avoid negative feelings, and wish everything would just be fine. They often try to act publicly like everything is fine, but they have no idea how to maturely process and learn from their negative feelings. Instead, they enter into an intra-psychic battle with their negative feelings, often working to banish them, or criticize themselves out of their feelings or try to “stay positive”. This creates a powerful “split” in their psychological systems. Namely, their feeling system is sending one signal, their internal narrator is in conflict with that signal, and they are trying to publicly present a totally different image than their inner conflict. All of this sets the stage for a “neurotic breakdown”.
In addition, I see many parents who value their kids, but who do not know how to guide their children in processing negative feelings. Instead, too many have been caught up in “self-esteem nation” and act in an overprotective way, essentially communicating both that their kids are fragile and that others are responsible for keeping you happy. Another group teaches their kids to repress and minimize their feelings. I am not blaming parents here. The modern world is complicated and psychologists and psychiatrists have generally not done a great job being clear about the nature of emotions and relational needs.

At the societal level, we need to recognize both the dramatic changes the information technological revolution has brought to our world and how many of the institutions that provided guidance for the good life are breaking down. Religious systems have lost much of their authority. The political system has broken down into a polarized way. I think our educational system is broken in the way it assesses performance and fails to teach character values. Science often seems to characterize the world as an amoral, meaningless physical system. In other words, in terms of our existential/transcendental understanding, there seems little that supports the deep-seated need that many people have for true meaning making. So, we live in a fast-paced, high-stress world in which we are overloaded with choice, we regularly observe massive amounts of inequity in power and resources, we give lip service to negative feelings but often characterize them as disease states and provide very little real education about human emotions and needs, and institutions that provided deep meaning making systems have lost their authority.
The bottom line is that depression arises, in most cases, when people do not receive the necessary psychological nourishment from their investments. This arises because of brutal environments and injury from traumas, diminished capacities to meet growth expectations, intrapsychic and interpersonal conflict with important others. Unable to find a path forward folks shutdown and, unfortunately, getting depressed in modern society likely creates more problems than it solves. So folks get trapped in neurotic depressive cycles.
There is clearly no easy fix, as depression is a massive health problem. But I do believe there is much that can be done. We need (and can achieve) a much better shared understanding of human psychological needs and nourishment. We also need a clear recognition from institutions like the World Health Organization that depression emerges as a function of psychological malnourishment, rather than being brain disease stemming from neurological malfunctions.
My ultimate vision is for the development of a holistic meaning-making system that harmonizes the natural sciences, the social sciences, and the humanities in a way that affords an understanding of our human natures such that we can have a more effective guide toward fulfillment during these rapidly changing times.
Gregg Henriques, Ph.D., author of A New Unified Theory of Psychology, directs the Combined Clinical and School Psychology Doctoral Program at James Madison University. He is a licensed clinical psychologist with expertise in depression, suicide, and the personality disorders. He has developed a new meta-theoretical system for psychology articulated in many professional journals and is now applying that system to researching well-being, personality, and social motivation, and he and his students are working on the development of a general system of psychotherapy. Henriques received his M.A. in Clinical/Community Psychology from UNC-Charlotte and his Ph.D. in clinical psychology from the University of Vermont. He also completed several years of post-doctoral training at the University of Pennsylvania under Aaron T. Beck exploring the effectiveness of various cognitive psychotherapy interventions for suicide and psychosis. Henriques teaches courses in personality theory, personality assessment, social psychology and integrative adult psychotherapy.