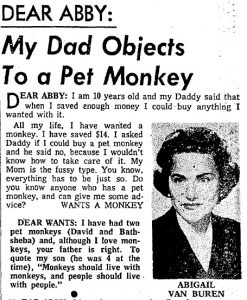
We all dish out opinions and advice whether asked for or not.
Much of it harmless; some, necessary and kind.
Then there’s those we dole out without knowing what the hell we’re talking about. Where we should tread carefully, we lumbar.
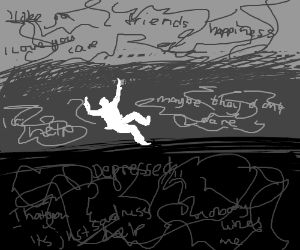
For better or worse, there’s tremendous power in words we use to express our opinions. When vulnerable – as we are during depression – the critical or misguided words of others take on the ring of gospel truth. Some may blame us for our depression.
In one poll, 54% of Americans said they thought of depression as a “personal or emotional weakness”. This explains much of stigma surrounding not only depression but all mental illness.
In a recent survey, what do 43.8 percent of women state as the Number 1 reason for not telling someone they were depressed?
“Others would think I am weak or think less of me.“
What do 57 percent state as their Number 1 reason?
“I believe I will get over it by myself”, followed by the same reason as women, the fear of being seen as weak, at 32 percent.
In the book, Unholy Ghosts: Writers on Depression, author Susanna Kaysen writes:
“The Failure of Will theory is popular with people who are not depressed. Get out and take your mind off yourself, they say. You’re too self-absorbed. This is just about the stupidest thing you can say to a depressed person, and it is said every day to depressed people all over this country. And if it isn’t that, it’s, shut up and take your Wellbutrin. These attitudes are contradictory. Conquer Your Depression and Everything Can Be Fixed by the Miracle of Science presuppose opposite explanations of the problem. One blames character, the other neurotransmitters. They are often thrown at the sufferer in sequence: Get out and do something, and if that doesn’t work, take pills. Sometimes they’re used simultaneously: You won’t take those pills because you don’t WANT to do anything about your depression, i.e. Failure of Will.”
Some just don’t think of it as the illness it is, but an excuse not to work hard.

Years ago, when I first told my three law partners that I was diagnosed with major depression and would need to take time off from work. They sat there stunned. After a moment of awkward silence, one partner said, “What in the world do you have to be depressed about? You’ve got a great job, wife, family and friends. Take a vacation!”
His anger humiliated me. “What’s wrong with me?” I thought.
I later learned that his reaction was, sadly, all too common. His judgment was that a lack of gratefulness was at the root of my distress. If only I jetted to Florida and sat under a palm counting my blessings, I would be depression-free.
For some time, these types of comments hurt me. They made me feel less-than. But after a while, they often made me angry. I thought, “What the hell do I have to do to be worthy of their mercy?” In retrospect, it wasn’t a question of my worthiness, but their ignorance. They didn’t have an emotional reference point for depression. They thought of it as stress, or, at worst, a bit of burnout. I recall a surgeon friend of mine (you would think that he, as a medically trained person, would know better!) telling me I was just in a “funk.” And then he said, “You want to see people who really have a right to be depressed? You should see the poor people with little money take two bus rides just to get to my office!”
Another painful innuendo. I had no right to be depressed, he must have thought. I was an upper-middle class professional, after all.
Some people (friends, family and business associates) will never be able to overcome the inertia of their own ignorance. They’re not bad people. It’s just the way life is. And we have to learn to be okay with that.
One of my best friends who has struggled with depression the past five years is frustrated by his wife’s lack of interest in talking to him about his depression. “Why doesn’t she love me, Dan?” “It’s not that she doesn’t love you,” I replied. “It might just be that she’s not capable of understanding in the way you want her to.”
But then there are others. These precious souls – and there don’t have to be lots of them – who have our back. They truly want to understand and help. Mother Teresa was once asked by a hard-boiled reporter what God expects of humanity. I think the reporter expected some stock answer. Mother Teresa, in all her gracious dignity, said that all God really wants from us to be is a “loving presence” to one another. There are those in our lives who want to be that presence to us.
Give them the chance to be that light.