We set our clocks back an hour in early November, resulting in shorter days, and darker skies before most of us leave work each afternoon.
We set our clocks back an hour in early November, resulting in shorter days, and darker skies before most of us leave work each afternoon.
It is important to understand the effect that light has on us. If you find yourself falling into the doldrums at this time of year as the number of daylight hours dwindle, seasonal affective disorder (SAD), sometimes called seasonal depression, may be to blame. Most SAD sufferers experience symptoms during the winter months, causing researchers to conclude that inadequate sunlight may play a role. But you don’t have to spend the winter months feeling depressed and unmotivated. Here’s what you need to know about SAD and how to alleviate it.
What Causes Seasonal Affective Disorder?
Most researchers believe decreased access to sunlight plays a role in seasonal affective disorder. Light affects our circadian rhythms, and UV rays can also change how the body processes vital minerals and other nutrients. For example, inadequate sunlight exposure is linked to low Vitamin D, which, in turn, has been linked to depression and other physical and mental health woes. So, the effects of darkness on the body—not just darkness itself—might be partially to blame.
A recent study, published in the Journal of Affective Disorders, bolstered the connection between SAD and inadequate sunlight. It found that weather and climate—including rain and pollution levels—don’t appear to alter mood. But access to sunlight is a major predictor of mental health. In the study, people who lived in regions with shorter, darker days were more likely to experience poor mental health.
While light almost certainly plays a role, not all cases of SAD occur during the short, dark days of winter. A small fraction of cases occur on a seasonal basis during the spring or summer, which suggests that no single factor can fully explain SAD. Other potential risk factors include:
- Seasonal lifestyle changes. If you only work during a portion of the year, have less to do during a specific time period, or face annual stress, you may experience seasonal depression.
- Seasonal associations with previous trauma and grief. Our minds form strong connections between the sights and sounds of seasonal shifts and memories of the past. You may find yourself growing depressed each year around the time you suffered a trauma or loss.
- Cultural norms and traditions. The high of the holiday season followed by the low of the new year can spur depression in some people.
- Certain health issues are more likely to manifest at specific times of the year. For example, if you have severe allergies, you may get depressed in the spring, while chronic bronchitis can make the winter months depressing.
Each of these factors alone is unlikely to trigger depression, but in conjunction with other risk factors—including a family history of any form of mental illness—they can lead to SAD.
Symptoms of Seasonal Affective Disorder
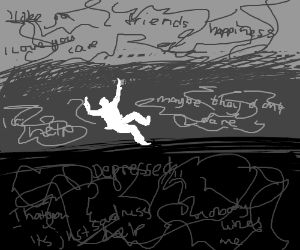
Cyclical depression that occurs around the same time each year or that relents when the season changes, is the hallmark of SAD. If symptoms are not cyclical, you might be diagnosed with another disorder, such as major depressive disorder or dysthymia.
People with SAD often experience depressive symptoms which are less severe than those associated with major depressive disorders. Though suicidal thoughts can and do occur—particularly if SAD is left untreated—these thoughts are less common. Some common symptoms include:
- Low energy, feelings of grogginess, or excessive sleep. People with summer SAD may experience insomnia.
- Changes in appetite. People with SAD are vulnerable to weight gain. SAD sometimes causes carbohydrate cravings, because carbs offer a temporary energy boost.
- Irritability and anger.
- Changes in your relationships with others: People with SAD often feel lonely and rejected.
- Loss of interest in previously enjoyed activities.
- Feelings of guilt.
- Dread or uncertainty about the future.
- Loss of motivation.
- Feelings of sadness.
Treatment for Seasonal Affective Disorder

People with winter SAD often respond well to light therapy, which involves sitting under a UV lamp for a short period of time each day. If you have access to daylight and can spend time outdoors, you might also find your symptoms improving if you receive 20-40 minutes of daily direct sun each day.
Treatment for major depression can also prove effective at treating SAD. Those treatment options include:
- Psychotherapy to help you talk through your feelings, identify problematic thought patterns, and more effectively cope with your depression. If causes relationship problems, therapy may also help improve your relationships. Your therapist can also talk to you about lifestyle changes—diet, exercise, activities—that may complement your treatment and help to alleviate your depression.
- Antidepressants: Depression alters chemicals in your brain. Sometimes lifestyle remedies are inadequate to get things back on track. Antidepressants can be effective and often need only to be taken for a short period.
Is It Possible to Prevent Seasonal Affective Disorder?
Research on the prevention of SAD is mixed. However, there is some evidence that light therapy can help prevent SAD in people with a previous history of the condition. If you’re worried that you might develop SAD this winter, talk to your doctor about preventative strategies. Also, maintain a healthy lifestyle—overeating during the holidays, excessive spending, and low motivation can all make SAD worse.
If you experience SAD, you don’t have to suffer through months of misery. SAD is one of the most treatable forms of depression, and with the right care, you can feel better in weeks, or even days.
This article originally appeared in Psychology Today magazine
Joel L. Young, M.D., is the Medical Director of the Rochester Center for Behavioral Medicine outside of Detroit and teaches Psychiatry at Wayne State University School of Medicine. Trained at the University of Michigan, Dr. Young is certified by the American Board of Psychiatry and Neurology and holds added qualifications in geriatric and forensic psychiatry. In addition, he is a diplomate of the American Board of Adolescent Psychiatry.
Dr. Young and his clinic have been primary investigators in a number of clinical trials involving antidepressant, AD/HD, and bipolar medications. He has authored three books and more than 70 textbooks and articles. His most recent book, When Your Adult Child Breaks Your Heart: Coping with Mental Illness, Substance Abuse, and the Problems That Tear Families Apart, was published by Lyons Press in December 2013.
References