Researchers have found that routine physically activity can help reduce depression. When you’re physically active your brain releases chemicals that help relieve stress, promote alertness, and improve your overall mental well-being.That said, becoming more physically active while fighting depression can seem daunting. Here are some simple tips to get you started and keep you going. Read the rest of this blog.
Five Simple Tips for Physical Activity While Fighting Depression
Shame: The Other Emotion in Depression and Anxiety
Psychologists have identified anywhere between 6 and 10 basic emotions experienced by humans. It will come as a surprise to no one that the primary emotion in depression is sadness and in anxiety fear. In all those case, feelings of sadness and fear combine to form a stew of toxic emotions. Read the rest of this blog.
Interview with Dr. John Greden, Director of the U. of Michigan Depression Center
Podcast: Play in new window | Download
 Today’s podcast interview is with Dr. John Greden, Professor of Psychiatry and Clinical Neurosciences in the Department of Psychiatry, Founder and Executive Director of the University of Michigan Depression Center, Founding Chair, National Network of Depression Centers. His research over the past 30 years has focused on studying biomarkers and developing treatment strategies to prevent recurrences of depression and bipolar disorders.
Today’s podcast interview is with Dr. John Greden, Professor of Psychiatry and Clinical Neurosciences in the Department of Psychiatry, Founder and Executive Director of the University of Michigan Depression Center, Founding Chair, National Network of Depression Centers. His research over the past 30 years has focused on studying biomarkers and developing treatment strategies to prevent recurrences of depression and bipolar disorders.
Listen to my interview with him on Itunes or Google Play.
Please note that it takes Apple and Google Play time to upload podcasts interviews. If this interview is not available, check back a little bit later.
Anxiety, Stress and Depression at All-Time High Among Americans: Study
Newsweek magazine reports that more Americans than ever before suffer from stress, depression, and anxiety, with those affected often too poor to afford general medical treatment, according to a new study which found that around 8.3 million people suffer from some form of serious psychological distress, which represents a large increase over previous years studied. Read the entire article here.
What It’s Like to Live With Both Anxiety and Depression
Blogger Jordan Ruhnke writes, “Living with depression feels like you’re in a dark hole with nowhere to go. Living with anxiety makes you feel like you’re losing your mind. Depression takes away all of your motivation and drive to do anything, but anxiety makes you want to constantly do that activity. Read the rest of her blog here.
6 Tips for Lawyers On Maintaining A Positive Outlook
Whether you’re Biglaw or SmallLaw or government law or stay-at-home-parent law, there are a few things that are important to pay attention to every day. Keeping a positive outlook is one of them. Attorney Garry T. Ross offers up some great ideas on how to do just that. Read his blog here.
15 Survival Tips for Anyone Living With a Mixture of Anxiety and Depression
Blogger Sarah Hughes writes, “I never got along with Anxiety, but my relationship with Depression was a whole different story. We despised each other. It was a deep loathing I had never felt before. We had formed a brutal rivalry, the only casualties on my side. It was every man for himself. Depression was a lot worse to me than Anxiety ever was. I think it’s because Depression had me brainwashed, kind of like the older guy you date in high school who you’re madly in love with, but he has you believing the entirety of your self-worth is dependent upon what he says.” Sarah recovered and offer these 15 tips. Read her blog.
These 11 Habits of People With Concealed Depression
Blogger Lexi Herrick writes, “Depression often goes unseen, unrecognized, and undiagnosed. A person with concealed depression is someone who is conditioned to deal with their inner demons in a way that doesn’t make them clearly visible. They may or may not be diagnosed, and this may or may not be something they’ve shared with even their closest of companions. The problem is that the world becomes darkest when we all stop being able to understand each other. We tend to believe that hardship is worn openly upon one’s chest like a battle scar, but many of these wounds do not easily reveal themselves to those that do not take the time to look.” Read the rest of her blog.
How to Prevent Stress From Shrinking Your Brain
 Have you ever felt so stressed out and overwhelmed that you can’t think straight? We now know that prolonged stress or trauma is associated with decreased volume in areas of the human brain responsible for regulating thoughts and feelings, enhancing self-control, and creating new memories. A new research study, published in today’s issue of Nature Medicine, is a first step in uncovering the genetic mechanism underlying these brain changes.
Have you ever felt so stressed out and overwhelmed that you can’t think straight? We now know that prolonged stress or trauma is associated with decreased volume in areas of the human brain responsible for regulating thoughts and feelings, enhancing self-control, and creating new memories. A new research study, published in today’s issue of Nature Medicine, is a first step in uncovering the genetic mechanism underlying these brain changes.
Depressed People’s Brains are More FragmentedIn this study, conducted by Professor Richard Dumin and colleagues from Yale University, scientists compared the genetic makeup of donated brain tissue from deceased humans with and without major depression. Only the depressed patients’ brain tissues showed activation of a particular genetic transcription factor, or “switch.” While each human cell contains more than 20,000 genes, only a tiny fraction of them are expressed at a given time. Transcription factors, when activated, act like light switches, causing genes to be turned on or off. This transcription factor, known as GATA1, switches off the activity of five genes necessary for forming synaptic connections between brain neurons. Brain neurons or nerve cells contain branches or dendrites that send and receive signals from other cells, leading to interconnected networks of emotion and cognition. The scientists hypothesized that in the depressed patients’ brains, prolonged stress exposure led to a disruption of brain systems involved in thinking and feeling. Depressed brains appeared to have more limited and fragmented information processing abilities. This finding may explain the pattern of repetitive negative thinking that depressed people exhibit. It is as if their brains get stuck in a negative groove of self-criticism and pessimism. They are unable to envision more positive outcomes or more compassionate interpretations of their actions.
Glucocorticoids Damage Brain Neurons
The stress response involves activation of a brain region known as the amygdala, which sends a signal alerting the organism to the threat. This results in activation of the HPA (hypothalamic-pituitary-adrenal) axis and release of a cascade of hormones, including cortisol, widely regarded as the quintessential “stress hormone.” While short-term cortisol release prepares the organism to sustain “fight or flight” and fend off an attacker, long-term exposure appears to cause brain neurons to shrink and interferes with their ability to send and receive information via branches called dendrites. In animal studies, under chronically stressful conditions, glucocorticoids such as cortisol can remain elevated for long periods.
Traumatic Experiences Can Shrink the Hippocampus in Those Who Don’t Recover
This finding is another piece of the puzzle regarding how stress and prolonged distress may impair our ability to think in creative and flexible ways. Research in both mice and humans has demonstrated an association between stress exposure (foot shock in mice, life events in humans) and shrinking of the hippocampus – the brain center responsible for forming new, time-sequenced memories. Studies in women with PTSD resulting from childhood sexual abuse and Vietnam veterans with PTSD have shown 12-26 percent decreases in hippocampal volume, relative to those without PTSD. In another study, patients recovered from long-term major depression showed a 15 percent decrease in volume of the hippocampus, compared to non-depressed patients.
Major Life Stress Damages the Prefrontal Cortex
In addition to hippocampal shrinkage, major life stress may shrink brain neurons in the Prefrontal Cortex (PFC), the brain area responsible for problem-solving, adaptation to challenge, emotional processing and regulation, impulse control, and regulation of glucose and insulin metabolism. In a study of 100 healthy participants conducted by Dr. Rajita Sinha and colleagues at Yale University, and published in the journal Biological Psychiatry, those with more adverse life events had greater shrinkage of gray matter in the PFC, compared to their less-stressed peers. Recent major life events, such as a job loss, make people less emotionally aware while life traumas, such as sexual abuse, seem to go further, in damaging mood centers that regulate pleasure and reward, increasing vulnerability to addiction and decreasing the brain’s ability to bounce back.
Summary
While the evidence is not yet conclusive, these studies suggest that prolonged exposure to stress can shrink the brain, both via the damaging effects of cortisol on brain neurons and by disrupting expression of genes that facilitate neuronal connections. This raises the question of whether there is anything we can do to prevent such damage. Since we can’t always control how much we are exposed to financial, relationship, or illness stress, are there preventive activities we can do to maintain cognitive resilience so we can continue to deal effectively with the stressors? It is not known if we can reverse the damage by these methods, but we may lessen it and make our brains more resilient to stress.
Brain-Enhancing Activities to Combat Stress
While the below list is not exhaustive, the three activities below have enhanced brain functioning in controlled studies.
Take a Daily DHA Supplement – DHA or Docosahexaenoic acid is an Omega-3 fatty acid that is a central building block of brain tissue. DHA is thought to combat the inflammatory effects of cortisol and the plaque buildup associated with vulnerability to Alzheimer’s disease. According to Dr. Mehmet Oz, in one study, a dose of 600mg of DHA taken daily for 6 months led the brain to perform as if it were three years younger.
Exercise Most Days – In studies with mice exercise led to a more improved performance on cognitive tasks than exposure to enriched environments with lots of activities and stimulation. Exercise leads to increases in BDNF or brain-derived neurotropic factor, a substance that strengthens brain cells and neuronal connections. BDNF is also thought to promote neurogenesis or the creation of new brain cells from existing stem cells in the hippocampus. Although these effects can’t be studied in living human brains, researchers have found increases in BDNF in the bloodstream of humans following workouts.
Do Yoga, Meditate, or Pray – These activities can activate what scientist Herb Benson at Massachusetts General Hospital calls “the relaxation response,” which lowers blood pressure and heart rate and lowers subjective anxiety. Benson and scientists from a genetics institute showed, in a recent study, that inducing the relaxation response can beneficially alter the expression of genes involved in inflammation, programmed cell death and how the body handles free radicals. The effects shown were in the same genes implicated in PTSD and depression. According to Jeffery Dusek, Ph.D., co-lead author of the study, “Changes in the activation of these same genes have previously been seen in conditions such as post-traumatic stress disorder; but the relaxation-response-associated changes were the opposite of stress-associated changes and were much more pronounced in the long-term practitioners.”
About the Author
Melanie Greenberg, Ph.D. is a licensed Clinical Psychologist and expert on Mindfulness and Positive Psychology. Dr. Greenberg provides workshops and speaking engagements for organizations, life, weight loss, or career coaching, and psychotherapy for individuals and couples. Visit her website: http://www.drmelaniegreenberg.biz
This article originally appeared in Psychology Today.
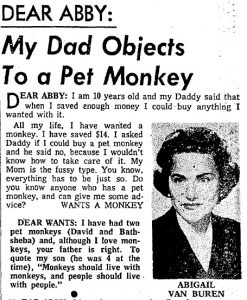
Other People’s Judgements About Our Depression
We all dish out opinions and advice whether asked for or not.
Much of it harmless; some, necessary and kind.
Then there’s those we dole out without knowing what the hell we’re talking about. Where we should tread carefully, we lumbar.
For better or worse, there’s tremendous power in words we use to express our opinions. When vulnerable – as we are during depression – the critical or misguided words of others take on the ring of gospel truth. Some may blame us for our depression.
In one poll, 54% of Americans said they thought of depression as a “personal or emotional weakness”. This explains much of stigma surrounding not only depression but all mental illness.
In a recent survey, what do 43.8 percent of women state as the Number 1 reason for not telling someone they were depressed?
“Others would think I am weak or think less of me.“
What do 57 percent state as their Number 1 reason?
“I believe I will get over it by myself”, followed by the same reason as women, the fear of being seen as weak, at 32 percent.
In the book, Unholy Ghosts: Writers on Depression, author Susanna Kaysen writes:
“The Failure of Will theory is popular with people who are not depressed. Get out and take your mind off yourself, they say. You’re too self-absorbed. This is just about the stupidest thing you can say to a depressed person, and it is said every day to depressed people all over this country. And if it isn’t that, it’s, shut up and take your Wellbutrin. These attitudes are contradictory. Conquer Your Depression and Everything Can Be Fixed by the Miracle of Science presuppose opposite explanations of the problem. One blames character, the other neurotransmitters. They are often thrown at the sufferer in sequence: Get out and do something, and if that doesn’t work, take pills. Sometimes they’re used simultaneously: You won’t take those pills because you don’t WANT to do anything about your depression, i.e. Failure of Will.”
Some just don’t think of it as the illness it is, but an excuse not to work hard.
Years ago, when I first told my three law partners that I was diagnosed with major depression and would need to take time off from work. They sat there stunned. After a moment of awkward silence, one partner said, “What in the world do you have to be depressed about? You’ve got a great job, wife, family and friends. Take a vacation!”
His anger humiliated me. “What’s wrong with me?” I thought.
I later learned that his reaction was, sadly, all too common. His judgment was that a lack of gratefulness was at the root of my distress. If only I jetted to Florida and sat under a palm counting my blessings, I would be depression-free.
For some time, these types of comments hurt me. They made me feel less-than. But after a while, they often made me angry. I thought, “What the hell do I have to do to be worthy of their mercy?” In retrospect, it wasn’t a question of my worthiness, but their ignorance. They didn’t have an emotional reference point for depression. They thought of it as stress, or, at worst, a bit of burnout. I recall a surgeon friend of mine (you would think that he, as a medically trained person, would know better!) telling me I was just in a “funk.” And then he said, “You want to see people who really have a right to be depressed? You should see the poor people with little money take two bus rides just to get to my office!”
Another painful innuendo. I had no right to be depressed, he must have thought. I was an upper-middle class professional, after all.
Some people (friends, family and business associates) will never be able to overcome the inertia of their own ignorance. They’re not bad people. It’s just the way life is. And we have to learn to be okay with that.
One of my best friends who has struggled with depression the past five years is frustrated by his wife’s lack of interest in talking to him about his depression. “Why doesn’t she love me, Dan?” “It’s not that she doesn’t love you,” I replied. “It might just be that she’s not capable of understanding in the way you want her to.”
But then there are others. These precious souls – and there don’t have to be lots of them – who have our back. They truly want to understand and help. Mother Teresa was once asked by a hard-boiled reporter what God expects of humanity. I think the reporter expected some stock answer. Mother Teresa, in all her gracious dignity, said that all God really wants from us to be is a “loving presence” to one another. There are those in our lives who want to be that presence to us.
Give them the chance to be that light.
Built by Staple Creative